Written by Alex Ramsey, instructor in the Department of Psychiatry at the School of Medicine
Implementation science has generally been viewed as the final step in the research translation process and only in the context of long-standing and well-validated interventions. There is reason to believe, however, that we should be considering implementation issues earlier in the research process. The translational research paradigm places discovery science and implementation science on opposite sides of the T0-T4 translational spectrum, with the assumption that, over time, research in a particular area will proceed stepwise from earlier to later stage translational purposes. The traditional thought is that implementation of an innovation into practice most aptly takes place after efficacy and effectiveness of an innovation has been established.

This widely accepted stepwise process has logical and intuitive appeal, as it ensures that implementation resources are not wasted on innovations that are untested, unproven, or ineffective. Only those demonstrating sufficient effectiveness or relative advantage are transferred into practice. Inherent within this paradigm, however, the approaches and methods of implementation science never cross paths with the “early stage” world of cutting edge precision medicine innovations—such as the development and testing of genomic applications and technology-based therapeutic tools—in which the evidence base on efficacy is still growing. Despite the potential of precision medicine innovations to radically improve patient engagement and treatment in behavioral health, there has been a notable lack of implementation research on the use of emerging and promising precision medicine discoveries.
Expanded role of implementation science
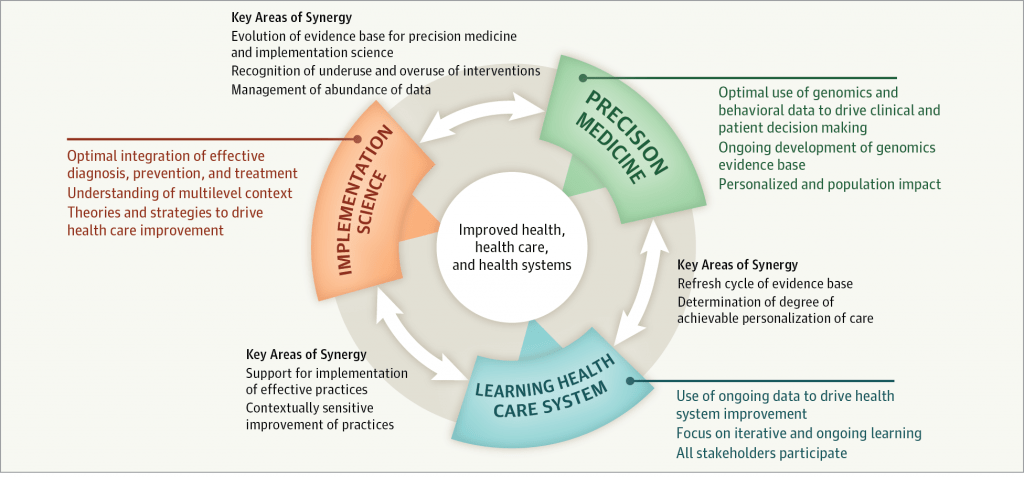
Despite its traditional role, implementation science is in a stage of “boundary spanning,” expanding its scope to create synergy with other fields with complementary perspectives. These fields include the precision medicine areas of (1) genomics, which remains ripe for preclinical and clinical discovery and (2) technology, which provides new platforms for delivering treatments that have been previously tested and validated in efficacy and effectiveness studies.
A key question in the behavioral health field is “Can the concepts, methods, and approaches of implementation science benefit the research-to-practice translation of these early stage research areas (e.g., precision medicine innovations) that have historically fallen outside the scope of implementation science?”
There is reason to believe that we should be considering implementation issues earlier in the translational research process, such as with precision medicine innovations for behavioral health.
A potential limitation of the traditional stepwise model is that it may slow the process of translating research into practice.
Although studying the implementation of a rapidly-emerging class of innovations such as genomics may have traditionally been viewed as controversial, the inadequate attention to implementation issues alongside utility/effectiveness testing may have contributed to the often-cited 17-year research to practice gap. Expanding the role of implementation science would push the envelope on how soon scientific advances can and should be implemented, at least on a small scale, to narrow the research to practice translational gap.
Benefits of “early stage” implementation efforts
The integration of precision medicine innovations into practice is still in its infancy, and ongoing scientific discoveries will continue to advance and refine our understanding of the role of genomic data, technology, and other innovations in behavioral health care. However, the unprecedented potential of these early stage innovations to engage populations and inform behavioral health care demands timely conduct of “early stage” implementation studies.
In addition to expanding the boundaries of implementation science, there are at least three potential benefits to considering implementation issues prior to the unequivocal establishment of innovation effectiveness:
- Accelerating the transfer of innovations into practice: Collecting data on implementation perceptions (e.g., attitudes) and resources (e.g., staffing) alongside effectiveness/utility testing will bring us to the point of system-ready innovations sooner than addressing effectiveness and implementation issues separately in a stepwise approach.
- Improving the design and packaging of innovations: Attending to feasibility and the innovation-organization fit through small-scale, early stage implementation efforts can ensure more usable and useful innovations and inform ongoing and necessary adaptations with greater efficiency.
- Refining organizational and system processes involved in implementation: Trialing implementation efforts, pilot testing implementation strategies, and modifying these approaches as the evidence base for the innovation evolves will better prepare the setting for implementation and ensure that the context is receptive for timely uptake of the innovation.
Potential approaches
There are a few general approaches that may help us to bridge the translational worlds of implementation science and early stage innovation discovery:
1) Designing for Dissemination (and Implementation):1 This involves improving the ways in which precision medicine innovations are packaged and presented to users (e.g., providers, patients) based on an understanding of the contexts in which they are to be implemented. This is best achieved when multiple stakeholders (e.g., technology developers, clinical leaders and staff, systems scientists) work together to align the content and format of the innovation with the goals and characteristics of the prospective adopting system.
2) Hybrid Effectiveness-Implementation Designs:2 This class of studies purposefully attempts to answer questions about both the effectiveness and implementation of an innovation. For example, we can compare two potential strategies for implementing a promising innovation and a comparison condition, such as through a 2 x 2 factorial design. This approach bypasses the stepwise model of addressing effectiveness and implementation research purposes separately. As such, these studies have the potential to speed the rate of eventual widespread implementation for promising yet unproven innovations.
3) Learning Mental Health Care System:3 This system is characterized by the efforts of more “nimble” behavioral health care agencies conducting continuous quality improvement and rapid cyclical tests of change to enhance translation of innovations into practice. Although not a universally accepted concept, research and practice can coexist, and this synergy can teach us new lessons about the pragmatic integration of behavioral health innovations in routine practice settings. Finally, an important reminder is that clinical research need not conclude once implementation research begins. As in the genomics field, although genomic innovations will slowly permeate behavioral health care practice as they are deemed to improve public health, discovery and early stage translational research can and should continue to advance the clinical utility of these innovations. When fully functional, the learning mental health care system will entail a bidirectional, cyclical translational process that creates rich practice-based evidence to inform early stage innovation development.
Summary
Implementation science may be able to help improve the integration of precision medicine and other early stage innovations within real-world practice. For good reason, the bulk of implementation research will always follow the establishment of effective interventions. However, implementation science is more than just a late stage consideration in behavioral health services research, and the field will likely benefit from thinking about implementation issues sooner in the process of translating behavioral health services research into practice.
Resources
Although not specific to behavioral health care, below are a couple of large-scale efforts to advance the implementation of early stage innovations, including personalized genomic data and other precision medicine applications, into health care.
- The Implementing Genomics in Practice (IGNITE) consortium
- The National Academies of Sciences, Engineering, and Medicine Roundtable on Genomics and Precision Health published a workshop summary entitled “Applying an Implementation Science Approach to Genomic Medicine”
References
1Brownson, R. C., Colditz, G. A., & Proctor, E. K. (2012). Dissemination and implementation research in health: translating science to practice. Oxford University Press.
2Curran, G. M., Bauer, M., Mittman, B., Pyne, J. M., & Stetler, C. (2012). Effectiveness-implementation hybrid designs: combining elements of clinical effectiveness and implementation research to enhance public health impact. Medical care, 50(3), 217.
3Chambers, D. A., Feero, W. G., & Khoury, M. J. (2016). Convergence of Implementation Science, Precision Medicine, and the Learning Health Care System: A New Model for Biomedical Research. JAMA, 315(18), 1941-1942.