Project Findings Lead to Two Years of NCI Supplement Funding
A project implemented through the Institute for Public Health’s Center for Dissemination & Implementation pilot and small grants program is making inroads in helping patients quit smoking.
Dr. Li-Shiun Chen, Associate Professor of Psychiatry and an Institute for Public Health scholar, has developed an implementation study which has decreased patient smoking rates from 57.4% to 54.3% by increasing the percent of patients receiving smoking cessation medication from 4.6% to 18.0%. In the study, a tablet-based assessment let doctors know which patients were interested in quitting. Based on the success of the tablet-facilitated assessment, Dr. Chen and her team have received funding from the NCI for a competitive supplement two-year grant: “Electronic Health Record (EHR)-enabled evidence-based smoking cessation treatment in cancer”.
Patients with severe mental illness have a much higher smoking rate than the general population. 60% of patients with severe mental illness smoke, compared to 20% of the general population. Despite these high smoking rates, few patients receive smoking cessation assistance from their doctors. There is an unmet service needs and great opportunity to provide patient-centered care. About 44% of smokers reported interest in taking smoking cessation medication, but only 13% of all smokers received medication treatment. Similarly, 25% of smokers reported interest in receiving smoking cessation counseling, but only 5.4% of all smokers received counseling.
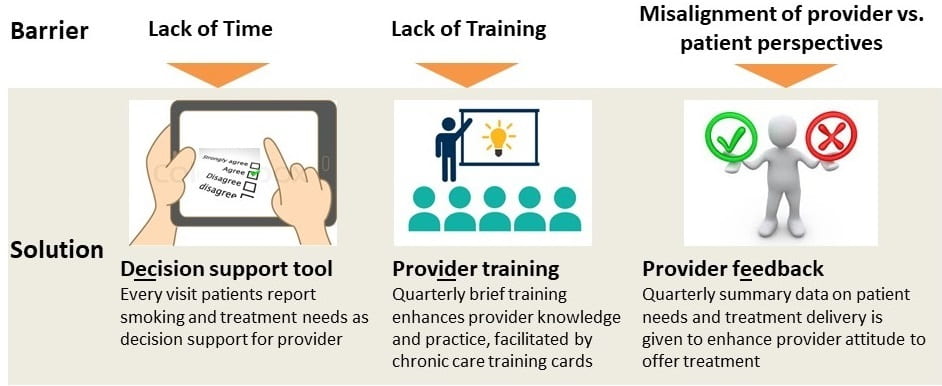
Dr. Chen aims to bridge the gap between doctors’ perceptions of a patient’s intention to quit and the patient’s actual intention. In assessing the patient’s intentions of quitting and interest in receiving cessation assistance, Dr. Chen’s team designed the tablet intervention, consulted with stakeholders on costs and intervention sustainability, and implemented the assessment intervention.
In order to gauge acceptability, they conducted key informant interviews with both patients and psychiatrists. The pilot data showed promising results for patients with severe mental illness seeking to quit or reduce smoking. Doctors and patients alike reported high acceptability (86% and 93%, respectively) of the tablet-based assessment. One provider said “[the tablet intervention] identified one patient who has previously been on the fence as being ready [to quit], which I may otherwise have missed.” Patient receipt of cessation medication jumped from 4.6% to 18.0%, and patient smoking rates decreased from 57.4% to 54.3%.

The tablet-facilitated assessment is a promising low burden strategy that can be easily integrated in many clinics. In fact, some primary care clinics – Siteman Cancer Center as one example – and a few Community Mental Health Clinics have expressed interest in Dr. Chen’s work and have agreed to collaborate with her team to assess the effectiveness, costs, and sustainability of implementing this practice.
_______________________________________
What: Underutilized evidence based practice: prescribing smoking cessation medication to patients with severe mental illness. Some patients who would benefit from smoking cessation medication are not being offered the medication.
How: How will we narrow the gap? Implementation Strategy: Tablet-based assessment of the patient’s intention to quit. This alerts doctors to patients interested in quitting and enables doctors to talk about medication with them.
Implementation Outcomes: Acceptability of the tablet-based assessment by doctors, medical staff, and patients.
Service outcomes: How effective was it in closing the gap between doctors’ perceptions and patents’ intentions to quit? Did that increase the proportion of patients receiving smoking cessation medication?
Patient Outcomes: Did more patients quit smoking?
Another aspect of the study which falls under Dissemination and Implementation Science is that there is engagement of stakeholders: doctors, patients, and medical staff, who gave input on the design of the tablet application and its incorporation into the psychiatry clinic.
The Center for Dissemination and Implementation pilot and small grants program at the Institute for Public Health supports the development of innovative projects by faculty scholars in order to help the project reach next-level, external funding.
Funding for this project is provided by the Institute of Clinical and Translational Sciences through the Clinical and Translational Science Award (CTSA) Program of the National Center for Advancing Translational Sciences (NCATS) at the National Institutes of Health, Grant Number UL1 TR000448.