Written by April Houston, MSW, MPH, communications assistant for the Institute for Public Health
Health care reform is in the news again (some would say it never left), as Republicans in the Senate have introduced a new bill to repeal and replace the Affordable Care Act (ACA), signed into law in 2010. Under the House’s version of the bill, known as the American Health Care Act (AHCA), the Congressional Budget Office estimates that over 20 million people will lose their health insurance by 2026. This worries public health experts for many reasons, but one concern that has not received much news coverage is the possible impact that the AHCA’s passage would have on the spread of HIV.
Institute faculty scholars Rupa Patel, MD, MPH, DTM&H, and Timothy McBride, PhD, MS, along with a team of infectious disease experts, medical professionals, health policy analysts, and social scientists in Missouri, Mississippi, Massachusetts, and Rhode Island, set out to investigate the link between an individual’s health insurance status and their utilization of pre-exposure prophylaxis (PrEP), a drug proven to prevent HIV transmission and thereby reduce HIV incidence. Their findings were recently published in the journal PLoS One.
Dr. McBride, a health economist, explained that their research had important implications for the ongoing health care reform debate as well as health care provision in general. “Affordability of medical care is an important aspect to measure when looking at the use of any service, especially when many of the people needing the service have low incomes and the costs of the services are high,” he said.
For the study, researchers analyzed 2014-2015 patient data from three PrEP clinics in St. Louis, Missouri, Jackson, Mississippi, and Providence, Rhode Island (201 patients total) to see what factors could predict whether or not patients who had been prescribed PrEP were taking it three months later. After controlling for age, race, education, income, and individual insurance coverage, they found that insured patients were four times as likely to use PrEP when compared to the uninsured. This result remained consistent when controlling for state Medicaid expansion and study site.
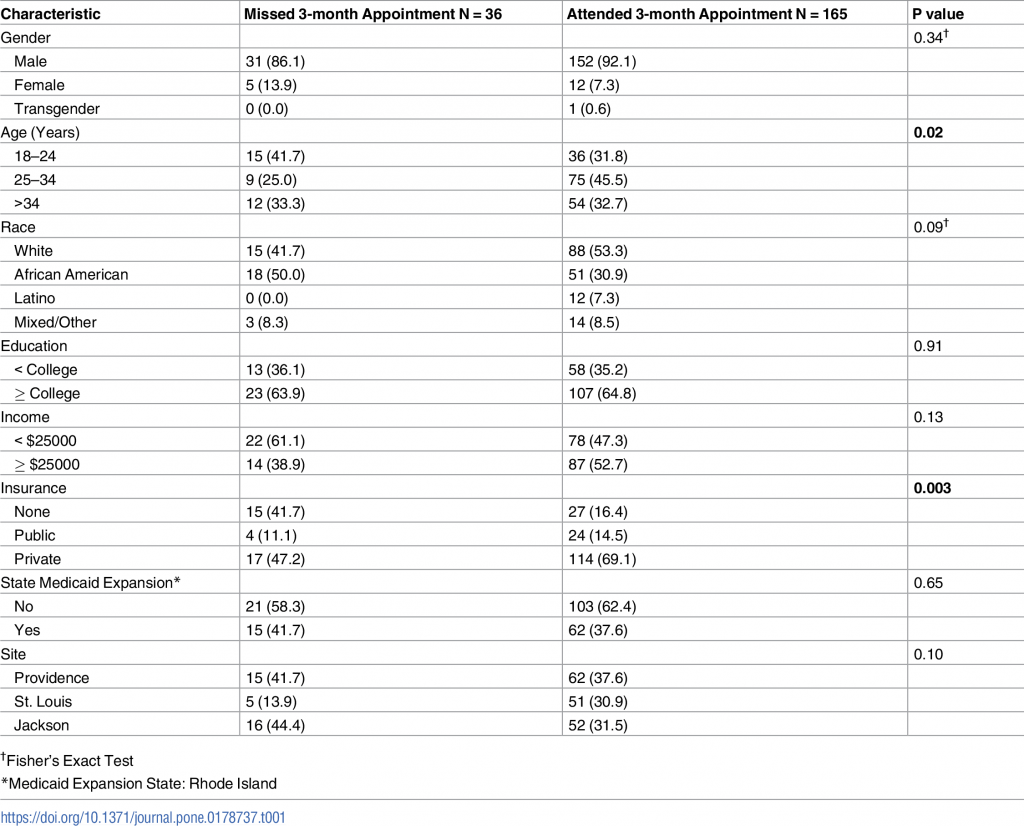
https://doi.org/10.1371/journal.pone.0178737.t001
In their article, the study team noted the relevance to the current health policy debate. “[ACHA] reforms… have the potential to change insurance access or quality of coverage to pay for PrEP-related care and costs for young adults, a group with high HIV incidence… Inadequate insurance coverage for at-risk individuals undermines the goal of reducing HIV incidence through PrEP and other preventative care.”
Dr. Patel recommended five concrete policy changes in light of their team’s findings: 1) insurance coverage should not be denied for those with pre-existing conditions (i.e. HIV), 2) public insurance coverage (i.e. Medicaid) should be preserved for those individuals who are currently enrolled in it, 3) Medicaid should be expanded in all 50 states, 4) essential benefits offered in employer-provided insurance coverage should not be reduced and should be made available to more people, and 5) federal subsidies and cost sharing payments should be preserved to ensure insurance coverage is affordable (i.e. lower copayments and deductibles for patients). “Currently, many of the people that need PrEP fall into the ‘gap’ group that is not eligible for Medicaid but also have no way of affording insurance coverage that allows access to PrEP care, which includes office visits, laboratories, and medications,” she said.
This research seems to indicate that an increase in the uninsured rate in the United States (particularly as a result of the proposed health care reform) could have dangerous consequences for the more than 1.2 million Americans estimated to be at risk for HIV.
For more information on this study, access the full report online here. St. Louis-area residents interested in PrEP or HIV testing or care can contact the Washington University Infectious Disease Clinic.
Dr. Patel’s research was partially funded by the Institute’s Public Health Cubed funding mechanism.