Written by Kim Furlow, communications manager for the Institute for Public Health
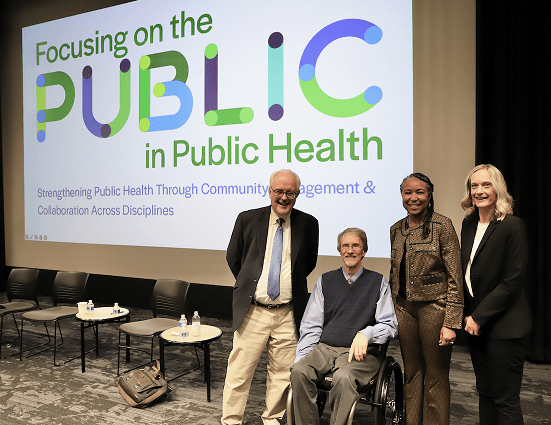
Attended by more than 400 students, faculty, university staff and community partners, the Public Health at WashU Annual Conference, “Focusing on the PUBLIC Health in Public Health” featured renowned public health experts along with faculty researcher panelists and their community partners all discussing solutions to critical public health issues facing our region and the world. For the first time in its 16-year history, the conference was expanded to two days in a collaborative effort between the Office of the Provost, WashU’s strategic vision—Here and Next, and the Institute for Public Health. In support of the University’s proposed new school of public health, the event is the first in a series of public health-related events to be produced through 2024.*
Day 1: Ushering in a new era of public health; health equity contradictions & a lower life expectancy
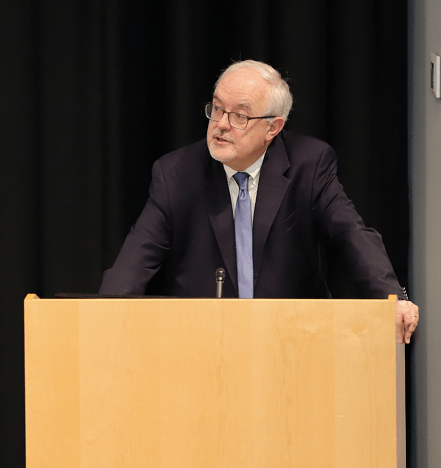
More than 100 guests including WashU Chancellor Emeritus, Mark S. Wrighton, PhD, National Council members, WashU public health faculty, students and St. Louis community members gathered at WashU’s Graham Chapel to hear opening remarks by William G. Powderly, MD, the Larry J. Shapiro Director of the Institute for Public Health, who discussed how WashU is expanding its public health stewardship here and across the globe.

As the university community looks toward the formation of a new school of public health, Vice Provost for Interdisciplinary Initiatives, Mary McKay, PhD reflected on the mission of the University strategic plan, Here & Next, which will mobilize research, education, and patient care to establish WashU and St. Louis as a global hub for transformative solutions to the deepest societal challenges. WashU continues to imbue its mission with health equity as a core value.
McKay introduced the evening’s keynote speaker, Darrell J. Gaskin, PhD, MS, director of the Hopkins Center for Health Disparities Solutions at Johns Hopkins Bloomberg School of Public Health, whose talk, “The Case for Health Equity”, fit perfectly with WashU’s equity focus.
Gaskin’s talk began with the fact that our nation’s life expectancy has lowered to age 76, the lowest in two decades. He spoke about how Americans tend to use language like the “deserving poor” to describe people who live in communities with safety net health providers, as if this is a positive way of describing the underserved and marginalized, who typically struggle to afford nutritious food, medication, and access to health care.
He added that in our nation, the cost of feeding the poor is equal to feeding the rich, and suggested that we focus on equitable outreach and the idea of “public health as a public good”. Gaskin touted Medicaid expansion as a “win-win” that provides support to the uninsured by incentivizing health care providers. He said we must offer medical care providers enough support to manage care delivery so that inequities (such as those perpetuated by the closing of hospitals in both urban and rural areas) are eliminated.
Gaskin closed by saying our nation’s approach to solving health inequities can be as simple as following the philosophical ethic of reciprocity, the Golden Rule: “Do unto others as you would have them do unto you.”
Safety nets are designed with holes in them, so people fall through!
Darrell Gaskin, keynote speaker

Moderated by Vice-Provost McKay, panelists Gaskin, Andwele M. Jolly, MHA, president and CEO of St. Louis Integrated Health Network and Heidi Miller, MD, chief medical officer at Missouri Department of Health and Senior Services, outlined their current work in service of public health. McKay asked their opinion on how WashU might assist with moving forward policy changes and queried their thoughts on the most important core elements of the proposed WashU School of Public Health.
Citing racism as an example of one of our nation’s most prominent public health threats, Andwele Jolly suggested facing it head-on, and he reiterated Gaskins’ point about treating others as we want to be treated. When referring to the newly proposed school, Jolly suggested including the voice of the community in WashU’s strategic approach, “using a listening ear” and incorporating what is heard. Miller concurred saying that Missouri is historically underfunded in public health so more funding is essential at all levels, especially on the economic front. Gaskin noted that WashU’s proposed new school might benefit from incorporating biostatistics and epidemiology into the curriculum taught systematically by expert faculty and including community involvement. “When community wins, the body of science wins,” Gaskin said.
The evening concluded with an audience reception alongside speakers and panelists.
Day 2: WashU interdisciplinary collaboration; “Public Health Matters”; and community partnerships with an impact!
Day two of the Public Health at WashU Annual Conference began with a warm welcome from Vice-Provost McKay, who discussed the proposed new school of public health and its values: Collaboration, real world impact, community centeredness, equity and social justice.

Left to right: Vice Provost McKay, School of Medicine Dean Perlmutter and Institute for Public Health Director Powderly offer day two opening remarks
McKay introduced the George and Carol Bauer Dean of the School of Medicine at Washington University, David H. Perlmutter, MD, who said that in a time when U.S. mortality rates are the highest ever and life expectancy is the lowest in two decades, the medical school is proving its “investment in better outcomes and improved care delivery”. He also alluded to public health’s link to medicine.
The work of public health, which must be inextricable from the work of academic medicine, is to ensure that we address all of the elements that make for a healthy life, and that we use our resources to help each and every member of our community live full and healthy lives.
David H. Perlmutter
Larry J. Shapiro Director of the Institute for Public Health, Bill Powderly offered a more extensive overview of some of the interdisciplinary research partnerships that help WashU stand out as a leader in public health stewardship. McKay then introduced renowned keynote speaker, the Dean and Robert A. Knox Professor of Boston University School of Public Health, Sandro Galea, MD, MPH, DrPH.

Galea led with his adoration for WashU and its strategic plan to add a proposed school of public health. “I can think of no better place than WashU to usher in public health and ensure that it matters in the coming decades.”
He alluded to the concept of fairness and whether or not institutions are teaching what this means. As an example, he discussed the deep health inequities that exist across the globe such as the ones plaguing those born in Nigeria, where life expectancy is only 54. He noted that between U.S. counties with the lowest and highest life expectancies, there is a 20-year age gap.

Galea discussed the fact that social determinants (zip code, access to health care, income level, etc.) contribute greatly to our life expectancy and today, are compounded by physical environment and poor health behaviors such as tobacco use and a lack of diet and exercise, among others.
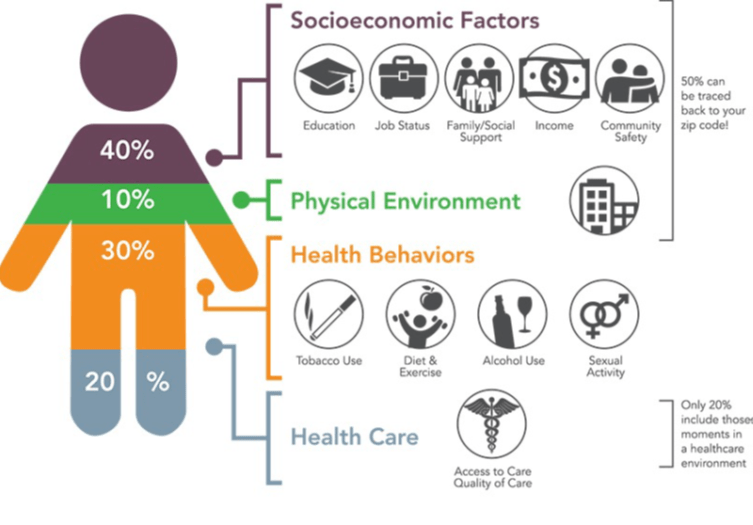
Galea cited studies showing that people with higher opportunities (such as living in the best zip codes, higher income levels, consistent access to health care) experience less health problems (20%) whereas 80% of the remainder of the studied population group remains at higher risk of chronic illness such as heart disease and diabetes.
Galea reiterated, “The problems of any of us are the problems of all of us.” The U.S. spends 40% more on health care than other wealthy nations & gets less out of it.”. He pointed to the skyrocketing rates of maternal mortality in the U.S. versus in other wealthier countries.
In addressing the pandemic, he discussed the three biggest causes:
1) Inequities: Some could work remotely, a large portion of the community’s frontline workers could not; those with lower-income occupations were hospitalized with severe illness or died at a higher rate than those with those in high-income jobs
2) Pre-existing poor health: Those with underlying conditions were most likely to be hospitalized and/or die, and;
3) Disinvestment in what could have helped: We did not protect people of color, frontline workers, who were the largest number of people lost during the pandemic
What’s next in health? Galea cited more allergens and more extreme weather will be of concern in the next 10 years. There were 1300 epidemic events from 2011-2017! More people (2/3 of the world) will be over age 65 by 2030.
Galea closed with an analogy to a goldfish in a fishbowl. Think of the goldfish as our health and think of its surrounding water as everything needed to keep the goldfish alive. How will YOU keep the goldfish healthy?
Two panels. One Idea. Cross-disciplinary and community partnerships can usher in health equity
The Public Health Conference featured two panel discussions. The first, Leveraging Community Collaboration & Research to Achieve Equitable Public Health, was moderated by Angela Brown, MD, professor of medicine at WashU’s School of Medicine and co-director of the Center for Community Health Partnership and Research.
Panelists included: Rev. Derrick Perkins, Sr., M.Div. | Centennial Christian Church
Susan Stark, PhD, OTR/L, FAOTA | School of Medicine, Washington University in St. Louis
Anneliese Stoever, MSW | St. Louis Area Agency on Aging
Sean Joe, PhD | Brown School, Washington University in St. Louis
Erise Williams, MPH | Williams and Associates, Inc.
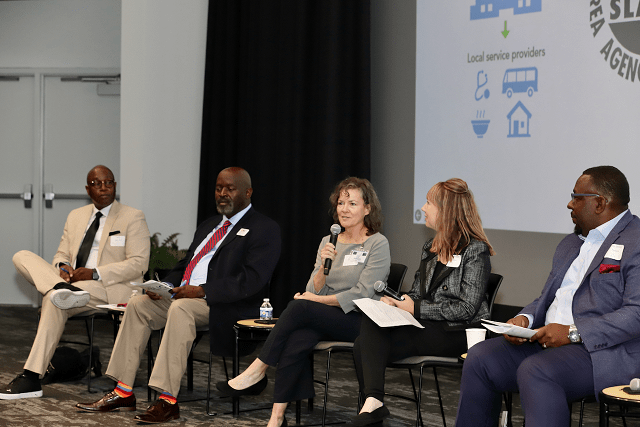
leveraging community -academic partnerships to foster health equity
The second panel, Public Health as a Cross-Disciplinary & Equitable Endeavor: Essential Needs & Concepts, moderated by Ross Brownson, PhD, the Steven H. and Susan U. Lipstein Distinguished Professor at WashU’s Brown School and School of Medicine, discussed the needs and concepts surrounding cross-disciplinary public health relationships.
Panelists:
Yusef Scoggin, MD | Covenant House-Missouri
Liz House, MPH | Perry County Health Department
Patty Cavazos-Rehg, PhD | School of Medicine, Washington University
Matthew Bernstine, AICP, LEEDAP | Sam Fox School of Design & Visual Arts, Washington University

Key Takeaways
- On forming community-academic partnerships: Do you know the community? Have you spent time there before offering expertise? The community knows what hurts. We need to manage our privilege. How can we serve them?
- Communication is key to community partnerships and sustainability in communities when the study ends! What’s working, what’s not in terms of incentives to participate…advocate, don’t manipulate! Invest to scale for transformative impact and population level results.
- The largest problem for diverse areas of STL is access to care. Largest number of overdoses are in south St. Louis City. We need more public health funding and community programs addressing social determinants of health.
- On the large divide between older/younger residents. How do we build community? Who is going to choose to live in this community? We need to plan for who will be the next to see communities survive.
- Why aren’t more people seeking mental health care? Stigma! We should think of mental health care like salt, sprinkling it everywhere, benefits, resources, providers where people are. We need more investment in and to retain our mental health care workforce.
- Drug overdose is the #1 cause of death in MO among those aged 18-44. Mobile app called uMAT-R helps individuals with substance use disorder. Clients who use the app see a significant decrease in substance use behaviors & an enhanced sense of support.
- How our community is designed affects how we live and whether or not we thrive. How do we experience our neighborhoods & how do they affect our health? Community development matters!
- Getting feedback from the community is the key to impactful public health!
The 2023 conference ended with a poster session on the conference theme and other public health-related topics.

For speaker bios and other information, read the 2023 Public Health at WashU Annual Conference program.
Members of the WashU and St. Louis community are invited to get involved with WashU’s new era in public health by engaging in the following requests and/or by attending future WashU public health-related events and activities.
- Nominate someone or apply for the 2024 William H. Danforth St. Louis Confluence Award
- Submit a nomination for dean. Learn more about the newly proposed school of public health and the dean search in this Record article.
- *Attend upcoming Public Health at WashU events and activities.
Photography by Tina McGrath